|
About Birth
Elective Induction of Labor
Table of Contents
“I live an hour from the hospital; if there’s a
blizzard, the road may be impassible.”
“I only get six weeks maternity leave. I don’t want
to get up from my desk to go to the hospital, but I don’t
want to sit home for two weeks either and only have four
weeks to recover.”
“My mother can come to help me out after the baby comes, but
she has to prearrange for the time.”
“If we induce labor, I can be sure of getting the doctor
that I really like.”
“I’m so huge and uncomfortable and tired of being pregnant.”
Who hasn’t heard one or more of these
nonmedical reasons for wanting to induce labor. Many
obstetricians have no objections to elective induction, and
some actually promote it: “We don’t want to let that baby
get too big” is probably the most common reason given,
although “impending post dates” gets my vote for most
creative indication. 36
The convenience of scheduling labor is even more of a boon
to busy obstetricians than to their patients, so if it
works and it’s harmless, why not induce?
To help your students make an informed decision, you must
have the facts about elective induction. Key, of
course, is whether it is generally safe and effective, but
in order to accurately weigh the risks and benefits, your
students will also need to know who makes a good candidate
and how to minimize the likelihood of problems.
Is
elective induction safe and effective?
The Food and Drug Administration and
the Physician’s Desk Reference, the bible of information on
drugs, recommend against elective inductions. 31, 35
The FDA “disallows” it; the PDR says,
“Since the available data are inadequate to evaluate the
benefits-to-risks considerations, Pitocin [the trade name
for oxytocin] is not indicated for elective induction of
labor.” By contrast, the American College of
Obstetricians (ACOG) includes “logistic factors” such as
“risk of rapid labor, distance from hospital, psychosocial
indications” on its list of indications for induction.
Inductions for these reasons would be elective inductions (ACOG
1999). 1
And, by ACOG’s lax standard, “tired of being pregnant” would
undoubtedly qualify as a “psychosocial indication.”
Problems with inductions stem from two
sources: the physiology of initiating labor and the side
effects of the procedures and drugs. First, despite
common belief that they can, obstetricians cannot switch
labor on at will. Starting and intensifying labor
involves a complex cascade of feedback mechanisms that
mutually reinforce and limit each other. It is an
elegant and delicate dance of hormones and other substances
between the baby, who initiates and controls the process,
and the mother. Dumping in oxytocin—with or without
cervical ripening procedures — often won’t initiate
progressive labor unless labor was on the verge of starting
on its own. This is the main reason why studies
consistently show that inducing labor, apart from the reason
for induction, considerably increases the likelihood of
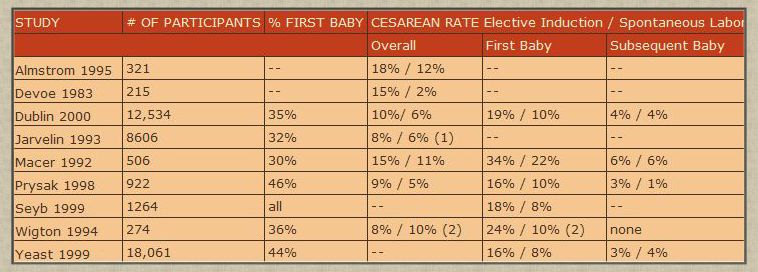
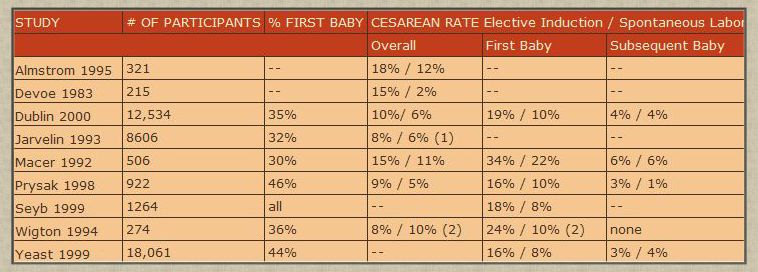
cesarean section in first-time mothers. 2, 8-9, 23, 28, 32, 36, 42, 45
(Some studies have concluded otherwise. The
reasons why are instructive and will be discussed in the
next section.) (See
Table.)
Second, all of the procedures and drugs used in inducing
labor can have adverse effects.
-
oxytocin (Pitocin, also called “Pit”):
-
uterine hyperstimulation:
Uterine hyperstimulation is a more common and serious
problem with inductions than when using oxytocin to
strengthen contractions in an already established
labor because it takes higher contraction pressures to
get and keep a labor going from a standing start.
20
Of ten studies comparing hyperstimulation rates at two
different oxytocin dosages, hyperstimulation rates
ranged from 2% to 60% at the lower oxytocin dose, and
six of the studies reported rates of 15% or more.
14
At the higher dose, hyperstimulation rates ranged
from 13% to 63%, and half reported that 25% or more of
the women experienced hyperstimulation.
-
fetal distress: Uterine
hyperstimulation can cause fetal distress.
Four studies reporting hyperstimulation rates also
reported fetal distress rates. 14
One reported an 8% rate at the lower dose; the rest
reported rates ranging from 15% to 54%.
-
low Apgar score: A separate
study reported that induction increased the percentage
of babies born in poor condition from 16% to 21%,
doubling the odds after statistical adjustment for
interdependent factors. 21
-
postpartum blood loss and
neonatal jaundice. 4-5, 7, 13, 16, 29, 37
Blood loss and jaundice may relate to direct effects
of oxytocin; increased use of IV fluids, especially IV
fluids that don’t contain salts; or both.
-
cesarean section: Oxytocin substantially increases
the likelihood of c-section in first-time mothers. (See
Table.)
-
procedures used with oxytocin:
Administering oxytocin requires an IV and electronic
fetal monitoring, which have their own potential adverse
effects. Because labor is more painful, women may
be more likely to want an epidural. One study comparing
first-time mothers having elective inductions with
first-time mothers beginning labor on their own reported
that having an epidural before 4 centimeters dilation
nearly quintupled the odds of cesarean, and they still
doubled with epidural placement at 5 centimeters or
more. 36
-
rupturing membranes:
Because amniotic fluid prevents umbilical cord
compression during contractions, rupturing membranes
increases the odds of episodes of abnormal fetal heart
rate and cesarean section for fetal distress. 12, 15, 28
This may be more of a problem during inductions because
contraction pressures are often higher. Since the
interval between rupture and birth may be long with an
induction, rupturing membranes increases the risk of
infection in women who subsequently have vaginal exams
and women colonized with group B strep. In rare
cases, it precipitates umbilical cord prolapse.
Cord prolapse is most likely when membranes are ruptured
early in labor when the head is still high, as would
happen with inductions.
-
prostaglandin E2 (trade
names: Prepidil, Cervidil): Prostaglandin E2, also
called dinoprostone, is inserted vaginally as a
gel (Prepidil) or as a removable tampon (Cervidil) to
soften the cervix. It can cause uterine
hyperstimulation and fetal distress. In some
cases, fetal distress can lead to cesarean section.
10
-
prostaglandin E1 (trade
name: Cytotec): Prostaglandin E1, more commonly
known as misoprostol is a tablet whose only FDA approved
use is as an oral medication for stomach ulcers. Its
manufacturer, Searle, does not formulate it for use in
labor and has repudiated its use for this purpose
because of safety concerns.33
The FDA says of Cytotec: 11
A major adverse effect of the obstetrical use of
Cytotec is hyperstimulation of the uterus which may
progress to uterine tetany [sustained contraction]
with marked impairment of uteroplacental blood flow,
uterine rupture (requiring surgical repair,
hysterectomy, and/or salpingo-oophorectomy [surgical
removal of ovaries and Fallopian tubes]), or amniotic
fluid embolism [very high maternal and fetal mortality
rate]. Pelvic pain, retained placenta, severe
genital bleeding, shock, fetal bradycardia
[dangerously slow fetal heart rate], and fetal and
maternal death have been reported. . . . The risk of
uterine rupture increases . . . with prior uterine
surgery, including Cesarean delivery.
Grand multiparity [several prior births] also appears
to be a risk factor for uterine rupture.
Unlike oxytocin, where the drip can be turned down or
off, Cytotec cannot be rescinded if it is causing
problems.
How did
obstetricians come to believe elective induction was
harmless?
-
belief that technology had
solved the problems with induction: The advent
of IV pumps to tightly control oxytocin dose and
prostaglandin gel to soften the cervix has led
obstetricians to believe that technology has conquered
the problems of uterine hyperstimulation and failed
induction. Obstetric philosophy and training
inculcates a preference for interventive management, so
once they stopped thinking that inducing labor had
serious consequences, induction rates were bound to
soar. In fact, hyperstimulation still frequently
occurs despite the pumps, and studies show that while
prostaglandin gel does an excellent job of softening the
cervix, it does little or nothing to reduce the cesarean
rate. 24, 30, 39
However, the preference for intervention and the belief
in its value blinds many obstetricians to those truths.
-
the norming of cesarean
section: The cesarean section rate has not been
below one woman in five since 1983. 40
After such an extended period, a rate in this range
feels normal, right, and unavoidable, although it is far
from that. If having many births end in c-section
isn’t seen as a problem, then the fact that inductions
lead to cesareans isn’t either.
-
the closure of the gap in
cesarean rates between induced and spontaneous labors:
The steep increase in cesarean rates has also
contributed to the illusion that induction no longer
matters. The gap between cesarean rates for
spontaneous and induced labors has closed because the
rate for spontaneous labors has risen to meet that of
induced labors. To illustrate, in a 1992 study,
researchers randomly assigned 3,400 women—two thirds of
them first-time mothers—to planned induction at 41 weeks
gestation or to await labor. 18
The women assigned to induction at 41 weeks were, in
effect, elective inductions since at the time, women
were not considered postdates until 42 weeks.
Twenty-one percent of the planned induction population
had cesareans versus 25% of the expectant management
group, leading the authors to conclude that planned
induction was the better policy. The study has
been cited since as an argument for elective
induction. But these were all healthy women with
full-term, singleton, head-down babies. In other words,
this was a population that should have been at minimal
risk for cesarean section.
A follow-up analysis reported
cesarean rates according to whether labor began
spontaneously or was induced. 19
Among first-time mothers, 26% of women beginning labor
spontaneously, whether in the planned induction or await
labor group, had cesareans. This rose to 30% of
women induced as planned and a whopping 42% of induced
women in the await labor group, of which only 17% were
done for abnormal fetal testing results. 18
By comparison, a study of 12,000 low-risk women
beginning labor at free-standing birth centers reported
a cesarean rate of 4% with 10% of first-time mothers
having cesareans. 34
-
bias toward intervention
over the natural process: The lead author of
the study above thinks that every woman should have a
cesarean as evidenced by her chairing a conference
entitled “Choosing Delivery by Caesarean: Has Its Time
Come?” 17
This goes a long way toward explaining why the main
paper misrepresents the true risks of induction and
ignores the appallingly high cesarean rates in both
spontaneous and induced labors.
The effect of obstetric bias can
also be seen in one of the studies in my table. Prysak
and Castronova compare outcomes in healthy mothers
having elective inductions matched to women beginning
labor spontaneously. 32
They conclude that elective induction is “safe and
efficacious” despite a cesarean rate of 16% for
first-time mothers having elective inductions versus 10%
for first-time mothers beginning labor on their own.
The authors favor elective induction as the following
passage from their introduction makes clear:
Advantages of elective induction include
patient-physician convenience, efficient use of
hospital personnel, and optimal time-of-day patient
care; unproved advantages include lowering the risk of
perinatal morbidity and mortality, birth trauma, and
cesarean delivery.
How did they make their data come out “right”?
They performed a logistic regression, a statistical
technique that accounts for confounding factors that may
obscure the true relationships among the issues of
interest. (An example of an appropriate use of logistic
regression would be accounting for other drug use and
cigarette smoking in cocaine users to get at the true
effect of cocaine on the baby.) Except that
Prysak and Castronova include the need for cervical
priming and the use of oxytocin in their regression,
which factored out the effect of induction on outcome.
Who
makes a good candidate for elective induction?
The ideal candidate for elective
induction is a woman who has given birth vaginally before,
whose cervix is ready for labor, and who has begun to
dilate. This, of course, is also a woman who will
almost certainly shortly go into labor on her own. In
descending order of probability of success would be a woman
with a prior vaginal birth or births whose cervix wasn’t
quite ready for labor, a first-time mother whose cervix was
ready to go, and a first-time mother with a long, firm,
closed cervix. A woman in the last category has truly
dismal chances for vaginal birth; as many as half of these
labors will end in cesarean section. 27
Perversely, though, if a woman’s doctor has a high cesarean
rate, inducing or awaiting spontaneous labor may not
matter. It will make no or only a small difference to
her chance of cesarean.
How can women considering elective induction minimize the
risks?
(adapted from The Thinking Woman’s Guide to a Better
Birth © 1999 by Henci Goer)
-
Refuse induction if you have
no prior births. Induction will increase the
chances of cesarean by anywhere from 50% to 250%. (See
Table.)
-
Refuse Cytotec (misoprostol,
prostaglandin E1). As noted above, Cytotec has a
propensity for precipitating women into short, violent
labors and a potential for catastrophic complications.
Cytotec was not formulated for use in inducing labor and
has not been approved by the FDA for this purpose,
although recently, lobbying by ACOG led the FDA to lift a
ban. Besides being riskier than Prepidil and Cervidil
(prostaglandin E2), Cytotec offers no compensating
advantages—at least not for women. Cytotec produces
virtually identical cesarean rates compared with
inductions involving prostaglandin E2. 22
The higher risks and equivalent effectiveness
notwithstanding, hospitals like Cytotec because it costs
mere pennies a dose compared with $75 to $100 dollars per
dose of prostaglandin E2. Obstetricians like it
because it allows them to practice “daylight
obstetrics”—insert the pill in the morning, return later
in the day for the delivery or the cesarean, be home in
time for dinner. 41
-
Refuse rupture of membranes before labor is
well-established and progressing. Having intact
membranes means you can back out if the induction doesn’t
work. Refusing early rupture also reduces the risk
of fetal distress from cord compression; the risk of
infection, which avoids IV antibiotics and septic workups;
and the rare but catastrophic risk of umbilical cord
prolapse.
-
Consider refusing induction
with an unready cervix and/or little or no dilation.
These conditions greatly increase the probability of
cesarean section regardless of the use of cervical
ripening procedures. 27, 43-44
-
When cervical ripening is necessary, request
Cervidil. Unlike Prepidil, it can be removed
should uterine hyperstimulation occur.
-
Avoid mechanical dilators for
cervical ripening. These materials gradually
dilate the cervix by absorbing water. They are not as
effective as prostaglandin E2 at either promoting
successful labor induction or achieving vaginal birth, and
they may increase the risk of infection. 25, 43 Again,
lower cost is the single advantage.
-
Although this should be
standard practice, make sure the IV fluid contains salts.
Salt-free fluids, especially in combination with oxytocin,
one of whose effects is fluid retention, can cause serious
blood-chemistry imbalances. 14
-
Have continuous electronic
fetal monitoring. It reduces the risk of
newborn seizures. 26
-
Insist on a low-dose(physiologic)
oxytocin regimen that allows at least 30 minutes between
dose increases. 14
The chance of developing adverse effects goes up with the
total amount of oxytocin given and the peak dose.
High-dose regimens greatly increase both.
-
Arrange to have the nurse try turning off the
oxytocin once active, progressive labor is established.
When labor kicks in, it may continue on its own without
the extra stimulus. This will be less painful for
you and easier on the baby. A plain IV will be kept
running, so oxytocin can easily be restarted if needed.
-
Low-dose, long-interval
protocols increase the odds of being able to turn the
oxytocin drip down or off in active labor.
3
-
Avoid or at least hold off on an epidural. Because
epidurals slow labor, they can substantially increase the
risk of cesarean section, especially when given early in
labor. Epidurals also cause fevers with prolonged
use. A fever in labor indicates a possible infection in
mother or baby and leads to a cascade of interventions.
-
Limit vaginal exams once
membranes are ruptured. There is a clear
relationship between length of time since rupture, the
number of vaginal exams, and infection. 38
-
Refuse internal
contraction-pressure monitoring. It
requires rupture of membranes, increases the odds of
infection, introduces risks of its own, and doesn’t
improve outcomes. 6
-
The discrepancy might have been greater had there been
more first-time mothers in the group.
-
10% is the primary cesarean rate at the study hospital
after removing cesareans for breech.
Bibliography
-
ACOG. Induction of labor. Practice Bulletin 1999, No
10.
-
Almstrom H, Granstrom L, and Ekman G. Serial antenatal
monitoring compared with labor induction in post-term
pregnancies. Acta Obstet Gynecol Scand 1995;74:599-603.
-
Blakemore KJ et al. A prospective comparison of hourly
and quarter-hourly oxytocin dose increase intervals for the
induction of labor at term. Obstet Gynecol
1990;75(5):757-61.
-
Buchan PC. Pathogenesis of neonatal hyperbilirubinaemia
after induction of labor with oxytocin. Br Med J
1979;2:1255-7.
-
Chalmers I, Campbell H, and Turnbul AC. Use of oxytocin
and incidence of neonatal jaundice. Br Med J
1975;2:116-8.
-
Chia YT et al. Induction of Labour: does internal
tocography result in better obstetric outcome than external
tocography? Aust NZ J Obstet Gynaecol 1993;33(2):159-61.
-
D’Souza SW et al. The effect of oxytocin in induced
labour on neonatal jaundice. Br J Obstet Gynaecol
1979;86:133-8.
-
Devoe LD and Sholl JS. Postdates
pregnancy. Assessment of fetal risk and obstetric
management. J Reprod Med 1983;28(9):576-580.
-
Dublin S et al. Maternal and neonatal outcomes after
induction of labor without an identified indication. Am J
Obstet Gynecol 2000;183:986-94.
-
Egarter CH, Husslein PW, and Rayburn WF. Uterine
hyperstimulation after low-dose prostaglandin E2
therapy: tocolytic treatment in 181 cases. Am J Obstet
Gynecol 1990;163(3):794-6.
-
FDA. Cytotec 2002.
-
Garite TJ et al. The influence of elective amniotomy on
fetal heart rate patterns and the course of labor in term
patients: a randomized study. Am J Obstet Gynecol
1993;168(6 Pt 1):1827-1832.
-
Gilbert L, Porter W, and Brown VA. Postpartum
haemorrhage—a continuing problem. Br J Obstet Gynaecol
1987;94:67-71.
-
Goer H. The Thinking Woman’s Guide to a Better
Birth. New York: Perigee Books, 1999.
-
Goffinet F et al. Early amniotomy increases the frequency
of fetal heart rate abnormalities. Br J Obstet Gynaecol
1997;104(5):548-53.
-
Goldberg CC et al. Effect of intrapartum use of oxytocin
on estimated blood loss and hematocrit change at vaginal
delivery. Am J Perinatol 1996;13(6):373-6.
-
Hannah, M. Choosing Delivery by caesarean: Has its
time come? Sponsored by the University of Toronto’s
Maternal, Infant, and Reproductive Health Research Unit at
The Centre for Research in Women’s Health, Toronto,
Canada, Nov 7, 2002.
-
Hannah ME et al. Induction of labor as compared with
serial antenatal monitoring in post-term pregnancy. A
randomized controlled trial. N Engl J Med
1992;326(24):1587-1592.
-
Hannah ME et al. Postterm pregnancy: putting the
merits of a policy of induction of labor into perspective.
Birth 1996;23(1):13-9.
-
Hauth JC et al. Uterine contraction pressures with
oxytocin induction/augmentation. Obstet Gynecol
1986;68(3):305-9.
-
Herbst A, Wolner-Hanssen P, and Ingemarsson I. Risk
factors for acidemia at birth. Obstet Gynecol
1997;90(1):125-30.
-
Hofmeyr GJ and Gulmezoglu AM. “Vaginal Misoprostol
for Cervical Ripening and Induction of Labour (Cochrane
Review).” In: The Cochrane Library, Issue 3, 2001.
Oxford: Update Software.
-
Jarvelin MR, Hartikainen-Sorri AL, and Rantakallio P.
Labour induction policy in hospitals of different levels of
specialisation. Br J Obstet Gynaecol
1993;100(4):310-315.
-
Keirse MJNC. Prostaglandins in preinduction cervical
ripening. Meta-analysis of worldwide clinical experience. J
Reprod Med 1993;38(1 Suppl):89-100.
-
Krammer J et al. Pre-induction cervical ripening: a
randomized comparison of two methods. Obstet Gynecol
1995;85(4):614-8.
-
MacDonald D et al. The Dublin randomized controlled trial
of intrapartum fetal heart rate monitoring. Am J Obstet
Gynecol 1985;152(5):524-539.
-
Macer JA et al. Elective induction versus spontaneous
labor: a retrospective study of complications and
outcome. Am J Obstet Gynecol 1992;166(6 Pt 1):1690-1697.
-
Mercer BM et al. Early versus late amniotomy for labor
induction: a randomized trial. Am J Obstet Gynecol
1995;173(4):1321-5.
-
Orhue AAE. A randomised trial of 45 minutes and 15
minutes incremental oxytocin infusion regimes for the
induction of labour in women of high parity. Br J Obstet
Gynaecol 1993;100:126-9.
-
Owen J et al. A randomized, double-blind trial of
prostaglandin E2 gel for cervical ripening and meta-analysis.
Am J Obstet Gynecol 1991;165(4 Pt 1):991-996.
-
Parke-Davis. Physician’s Desk Reference. 52d ed.
Montvale, NJ: Medical Economics Company, Inc., 1998.
-
Prysak M and Castronova FC. Elective induction versus
spontaneous labor: a case-control analysis of safety and
efficacy. Obstet Gynecol 1998;92(1):47-52.
-
Reuters Health. “Off-label Cytotec Use for Labor,
Abortion Prompts Searle Letter to Physicians.” Aug 29,
2000.
-
Rooks JP et al. Outcomes of care in birth
centers: the National Birth Center Study. N Engl J Med
1989;321(26):1804-1811.
-
Rooks JP. Midwifery and Childbirth in America.
Philadelphia: Temple University Press, 1997.
-
Seyb ST et al. Risk of cesarean delivery with elective
induction of labor at term in nulliparous women. Obstet
Gynecol 1999;94(4):600-7.
-
Singhi S et al. Iatrogenic neonatal and maternal
hyponatraemia following oxytocin and aqueous glucose infusion
during labor. Br J Obstet Gynaecol 1985;92:356-63.
-
Soper DE, Mayhall CG, and Dalton HP. Risk factors for
intraamniotic infection: a prospective epidemiologic
study. Am J Obstet Gynecol 1989;161(3):562-6.
-
Trofatter KF. Endocervical prostaglandin E2 gel for
preinduction cervical ripening. Clinical trial results.
J Reprod Med 1993;38(1 Suppl):78-82.
-
United States 1996. Month Vital Stat Rep 1997;46(1 Suppl
2).
-
vigilante obstetrics. Presented at Celebrating the Gift
of Birth, sponsored by the International Cesarean Awareness
Network, Cleveland, OH, Apr 20-22, 2001.
-
Wigton TR and Wolk BM. Elective and routine induction of
labor. A retrospective analysis of 274 cases. J Reprod Med
1994;39(1):21-26.
-
Williams MC, Krammer J, and O’Brien WF. The value
of the cervical score in predicting successful outcome of
labor induction. Obstet Gynecol 1997;90(5):784-9.
-
Xenakis EM et al. Induction of labor in the
nineties: conquering the unfavorable cervix. Obstet
Gynecol 1997;90(2):235-9.
-
Yeast JD, Jones A, and Poskin M. Induction of labor and
the relationship to cesarean delivery: a review of 7001
consecutive inductions. Am J Obstet Gynecol 1999;180(3 Pt
1):628-33.
© 2002
by
Henci Goer
article
reprinted with permission

Henci
Goer is an award-winning American author and internationally-know
who writes about pregnancy and childbirth from an evidence-based
perspective. She is the author of The Thinking Woman's Guide to a
Better Birth. Her previous book, Obstetric Myths Versus Research
Realities, is a highly-acclaimed resource for childbirth
professionals. An independent scholar, she is an acknowledged expert
on evidence-based maternity care. Goer has written consumer
education pamphlets and numerous articles for magazines as diverse
as Reader's Digest and the Journal of Perinatal and Neonatal
Nursing.
|