|
Ask The
Professional
What Is Herpes Simplex
2?

I have an inquiry of a
sensitive nature. What is Herpes Simplex 2? As a doula
and childbirth educator I would like to be more informed on this
subject for my clients.
Thank-you ! Elizabeth Lugmayer
Thanks
for asking about this, Elizabeth. Herpes is much more common than is
generally known. Many of my home birth clients had it. Groups
of people you least expect will carry it.
The
following composition compiles current information that includes
diagnosis and remedies. Hopefully it's easy for the novice as
well as the experienced clinician to embrace.
~Susan Oshel~
What Is Herpes?
There
are two strains of the HSV (Herpes Simplex Virus), 1 and 2. They are
both from the herpes virus family, herpesviridae, which causes
infections in humans.
Oral herpes (HSV-1) causes cold sores around the mouth or face.
Genital herpes (HSV-2) affects the genital area.
Herpes is one of the most common viral infections known to man,
affecting more than 80% of the population at one time or another,
including more than 20% of pregnant women.
Herpes Simplex Virus 2 is transmitted primarily by contact with
genital secretions. Public Health studies show that within
the United States, 10 to 40 million people carry the HSV-2 virus.
Many genital infections also carry a mixture of HSV-1 and HSV-2.
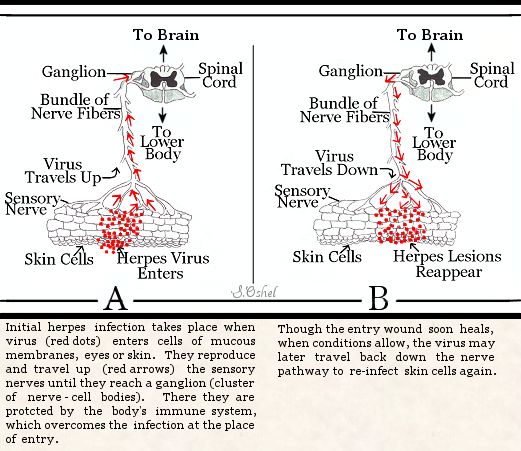
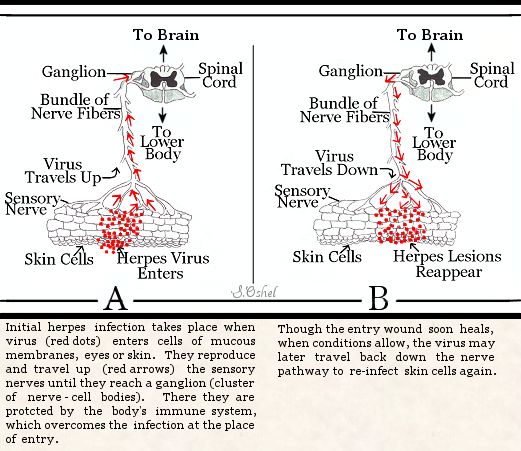
HSV interacts with epithelial or neuroepithelial cells and neurons.
The incubation period is between 2 and 4 weeks. During the initial
infection, HSV migrates to one or more sensory nerve ganglia, where
it remains latent and dormant indefinitely. An intact immune system
cures the infection at the portal (place of entry on the skin where
the fluids touched). The primary infection involves mucocutaneous
cells; recurrent infection involves stratified epithelial cells.
HSV is diagnosed by cytologic testing and microscopic examination. A
papanicolaou smear of the lesion shows multinucleated giant cells
with ground-glass nuclear appearance and cervical dysplasia. A
wet-mount preparation of lesion secretions reveals polymorphonuclear
leukocytes.
In many instances, your healthcare professional is able to make the diagnosis of
herpes from physical appearance of the lesions and no tests are
required. If your healthcare professional is not 100% certain, however, then fluid
from the blisters can be removed and tested for the herpes simplex
virus. This can be done through viral cultures which is very
accurate but generally takes 2 to 3 days to get the results and make
an official diagnosis. Another more immediate, but less accurate,
approach is to do a Tzanck test of the skin lesions. This involves
taking a sample of fluid from the blisters, staining the fluid with
a dye, and examining the stained fluid under the microscope looking
for a characteristic appearance of the virus. Finally, there is a
blood test that may be helpful for making a diagnosis, especially if
herpes simplex is suspected but no symptoms are present or if a
distinction between HSV-1 and HSV-2 is needed.
HSV infections may involve external genitals, the vaginal canal and
cervix. Symptoms are more pronounced with first infections of HSV.
Painful blisters form, rupture, and then drain, leaving shallow
ulcers that crust over and disappear after 2-6 weeks. A vaginal
discharge is seen if the cervix or vaginal mucosa is involved. The
woman may have fever, malaise, anorexia, painful inguinal
lymphadenopathy (disorder of the lymph nodes or vessels in the
groin), dysuria (painful urination), and dyspareunia (an abnormal
condition of painful intercourse for women).
Some people have no symptoms. Others get sores near the area where
the virus has entered the body. They turn into blisters, become
itchy and painful, and then heal. The virus can be dangerous in
newborn babies or in people with weak immune systems.
Most people have outbreaks several times a year. Over time, you get
them less often. Medicines to help your body fight the virus can
help lessen symptoms and decrease outbreaks. Correct usage of latex
condoms can reduce, but not eliminate, the risk of catching or
spreading herpes.
Once you have herpes, it is likely to recur. In between herpes
outbreaks, the virus lies dormant (like it is hibernating or
sleeping) in nerve cells. Recurrent HSV-1 infections on the lip are
often mild and are commonly referred to as cold sores or fever
blisters. HSV-2 lesions tend to recur more often and to be more
severe than HSV-1 infections.
The
virus can be reactivated due to "stressor stimuli's" such as fever,
another infection and the effects of other illnesses such as cold
and influenza, intercourse, menstruation, emotional and physical
stress, exposure to bright sunlight, gastric upset, fatigue or
injury, consequently resulting in the appearance of surface sores.
Repeated occurrences may result in keratitis (inflammation of the
cornea), encephalitis (inflammation condition of the brain), and
possible cervical carcinoma. These possibilities are rare. Most
recurrences tend to be milder and shorter in duration.
The infection may not show symptoms for a long time, and then become
activated by the aforementioned stressors and weakened immune
system. Most people have outbreaks several times a year. Over time,
you get them less often. Medicines to help your body fight the virus
can help lessen symptoms and decrease outbreaks. Correct usage of
latex condoms can reduce, but not eliminate, the risk of catching or
spreading herpes.
Women who have a history of genital herpes often wonder whether or
not it is safe for them to deliver their baby naturally. The good
news is most women with genital herpes will be able to deliver their
baby safely without the need for a cesarean section, provided their
disease is long standing and they do not have any active lesions at
or near term.
The pregnancy effects of a primary genital herpes infection (the
first incidence of an outbreak in pregnancy) include
miscarriage, preterm labor, and intrauterine growth retardation (IUGR).
The likelihood of problems increase with a “first outbreak”
occurring later in pregnancy. The frequency and severity of
recurrent infection also seem to increase with gestational age.
The route of HSV from mother to baby is via an infected birth canal
during birth. The risk of maternal-infant transmission is greater
during a primary infection than during a recurrent episode. Cesarean
birth is no longer recommended for all mothers with HSV because
transplacental infection can occur. Only those mothers with clinical
evidence of active lesions should give birth abdominally.
Babies of mothers with long-standing herpes infections have a
natural protection against the virus. Herpes antibodies in the
mother's blood cross the placenta to the fetus. These antibodies
help protect the baby from acquiring infection during birth, even if
there is some virus in the birth canal. That's the major reason that
mothers with recurrent genital herpes rarely transmit herpes to
their babies during delivery. Even women who acquire genital herpes
during the first two trimesters of pregnancy are usually able to
supply sufficient antibody to help protect the fetus.
If you are pregnant and know you have genital herpes, that fact
alone gives you a significant advantage in protecting your baby.
Studies show that most cases of neonatal herpes occur in babies
whose mothers don't have any idea they are infected.
Although genital herpes is common, the risk of your baby being
affected by neonatal herpes is low particularly if you contracted
genital herpes before the third trimester of pregnancy. In the USA
one in 1800-5000 live births are affected, in the UK one in 60 000,
in Australia and France one in 10 000 and in the Netherlands one in
35 000 are affected. This means that the majority of women with
genital herpes give birth to healthy babies.
For the babies who do contract the disease, fetal and neonatal effects can be serious. Microcephaly, mental
retardation, retinal dysplasia, patent ductus arteriosus and
intracranial calcification are sequelae. The signs include lethargy,
poor feeding, jaundice, bleeding, pneumonia, convulsions,
opisthotonus, bulging fontanelles, and skin and mouth lesions.
Neonatal infections with disseminated disease results in 82%
mortality. Survivors have CNS (central nervous system disorder) or
ocular problems in the first 5 years of life.
Neonatal herpes is not a reportable disease in most states, so there
are no hard statistics on the number of cases nationwide. However,
most researchers estimate between 1,000 and 3,000 cases a year in
the United States, out of a total of 4 million births. To put this
in greater perspective, an estimated 20-25% of pregnant women have
genital herpes, while less than 0.1% of babies contract an
infection. "Neonatal herpes is a remarkably rare event", says Zane
Brown, MD, an expert on neonatal herpes and a member of the
Department of Obstetrics and Gynecology at the University of
Washington. "Compared to all the other possible risks in a
pregnancy, the risk of neonatal herpes is extremely small."
"I think it's perceived to be more of a problem than it is", says
Scott Roberts, MD a researcher in the Department of Maternal Fetal
Medicine at the University of Kansas. "The rate of neonatal herpes
is very low, even though the prevalence of genital herpes in our
country is quite common."
Herpes can also be spread to the baby in the first weeks of life if
he or she is kissed by someone with an active cold sore (oral
herpes). In rare instances, herpes may be spread by touch, if
someone touches an active cold sore and then immediately touches the
baby. Babies who contract herpes neonatally can become very ill. It
is a greater risk in the first three months after birth. A newborn
baby can be infected from both forms of herpes 1 and 2. Therefore,
caution in handling the newborn is important even if you only have a
mouth sore, HSV 1. If a baby contracts HSV 1 from a sore that the
mother or father has (which can be transmitted by kissing), the
effects are seen after an incubation of 7 days. The baby will have
painful, swollen, reddened, sometimes bleeding gums with tiny
blisters on it's tongue, gums, lips and around it's mouth leaving
sores that heal within a week. They can also have a low grade fever,
be irritable and loose their appetite. Breastfeeding becomes very
difficult and often these babies are supplemented because they
cannot nurse due to pain in their mouths and depressed appetites. If
a baby contracts HSV 2 in the first three months after birth,
pneumonia also becomes a risk.
Keep in mind that there are precautions that can be taken to lower
the risk of transmission from mother to baby. It is mainly the
"unknown" infections that are transferred.
"The vast majority of babies born to mothers with genital herpes are
healthy, happy babies." American Social Health Association, 1996
Treatments
The following allopathic medications (as well as natural remedies)
carry various risks. Each will be a treatment of choice for some people and not for
others. Weighing the risk of the condition with the risk of the
treatment is important. In my walk as a midwife over the
past 30 years, I grew in the knowledge that "one size does not fit
all". I learned that we break all the rules! Though I
reverently question the side effects of medications, the side effects of the disease
are sometimes far more severe and should be judged on an individual
basis. Following is a full spectrum of treatments for herpes.
Prescriptive
Treatments:
Antivirals
Antivirals are the most commonly prescribed medication for treating
herpes. Antivirals can be topical (applied to the skin) or taken
internally to help suppress future outbreaks. Antiviral medications
are generally used to shorten the length of an outbreak and reduce
the number of outbreaks a person will experience. Antiviral therapy
can be taken as “episodic treatment” or as “suppressive therapy.”
Following are antiviral prescriptive medications:
Valacyclovir
A newer drug, valacyclovir (brand name Valtrex®), actually uses
acyclovir as its active ingredient. This medication delivers
acyclovir more efficiently so that the body absorbs much of the
drug, which has the advantage of taking the medication fewer times
during the day. It is the most commonly recommended drug for
pregnant women.
Acyclovir
The oldest antiviral medication for herpes is acyclovir. Acyclovir
is available as a generic drug and is also sold under the brand name
Zovirax®. It has been available since 1982 in a topical form (as an
ointment) and sold since 1985 in pill form. Acyclovir has been shown
to be safe in persons who have used it continuously (every day) for
as long as 10 years.
Famciclovir
Famciclovir (brand name Famvir®) utilizes penciclovir as its active
ingredient to stop HSV from replicating. Like valacyclovir, it is
well absorbed, persists for a longer time in the body, and can be
taken less frequently than acyclovir.
Numerous studies suggest that treatment of genital herpes infections
during pregnancy with the antiviral acyclovir is safe even during
the first trimester. There have been long term studies that suggest
the long term use of acyclovir during pregnancy is safe. Thus this
drug may be used in certain circumstances to prevent a break out
during pregnancy.
Following is a study done by the Department of Obstetrics and
Gynecology, University of Washington, Seattle, USA.
OBJECTIVE: The purpose of this study was to assess the efficacy of
acyclovir in the reduction of herpes simplex virus culture and
polymerase chain reaction positivity and cesarean delivery. STUDY
DESIGN: Women with recurrent genital herpes simplex virus were
randomized to acyclovir 400 mg three times daily or placebo from 36
weeks of gestation until delivery. A subset of daily specimens for
herpes simplex virus culture and DNA polymerase chain reaction was
self-collected. Analyses used chi(2), Fisher exact, and Mann-Whitney
U tests. RESULTS: Lesions occurred at delivery among 11 of 78 women
(14%) who received placebo and 4 of 84 women (5%) who received
acyclovir. Herpes simplex virus culture and polymerase chain
reaction positivity near delivery occurred in 7% and 34% women in
the placebo group and 0 and 2% in the acyclovir group. Cesarean
delivery for herpes simplex virus occurred in 8 of the women (10%)
in the placebo group and in 3 of the women (4%) in the acyclovir
group. Despite reductions in herpes simplex virus detection, 6% of
the women who received acyclovir had herpes simplex virus detected
by polymerase chain reaction on >20% of days. Neonatal outcomes were
similar between groups.
STUDY CONCLUSION: Acyclovir significantly reduced, but did not
eliminate, herpes simplex virus lesions and detection in late
pregnancy.
Vaccine research
Herpevac, a vaccine for HSV-2 is currently (as of February 2007)
undergoing clinical testing in women in the United States and
Canada. Previous studies have determined that this vaccine is
approximately 70% effective in women, but does not prevent the
disease in men.
Non Prescriptive Treatments:
Nutrition and Dietary Supplements
Lysine
Although the research to date is not entirely conclusive, lysine
supplements have been used to help treat or prevent mouth and
genital lesions caused by herpes. Supplementation of Lysine has
demonstrated the ability to reduce the duration of infection through
inhibiting the replication of the HSV. Taking lysine supplements or
increasing lysine in your diet (from foods like fish, eggs, and
potatoes) may speed recovery time and reduce the chance of recurrent
breakouts of the herpes infection. However, consuming foods high in
arginine (such as nuts or peanuts) may interfere with the
therapeutic use of lysine
Propolis
Propolis, a resin from tree bark and leaves, is loaded with
flavonoids (antioxidants that help fight infection and boost immune
function). A study of a small number of people with genital herpes
compared an ointment made from propolis to acyclovir ointment (a
medication outlined above commonly used for herpes). In this
research trial, the lesions of those using the propolis healed more
quickly than those using acyclovir. Research on larger numbers of
people would be helpful. In the interim, it may be worth trying
propolis ointment for genital herpes lesions if your doctor
approves.
Spirulina
Test tube studies suggest that spirulina, also known as blue green
algae, has activity against certain viruses including herpes.
Whether this laboratory finding will prove beneficial for people in
treating herpes infections is not known. More research is needed
before a recommendation can be made.
Vitamin
C and herbs
Tinctures of echinacea, siberian ginseng and reishi mushroom
combined 1-2 droppersful every 2 hours; vitamin C and zinc to body's
tolerance; lots of fluids to flush the system
Zinc
Topical preparations of zinc have shown benefit in relieving
symptoms and preventing recurrences of oral herpes lesions.
Herbs
The use of herbs is a time-honored approach to strengthen the body
and treat disease. Herbs, however, contain active substances that
can trigger side effects and interact with other herbs, supplements,
or medications. For these reasons, herbs should be taken with care
and only under the supervision of a practitioner knowledgeable in
the field of herbal medicine.
Teas
Lemon
balm (melissa) tea, also chamomile tea, hops, passionflower, st.
john's wort...tension tamer are all teas that calm the nerves. I've heard
some people using chamomile tea bags topically too.
Aloe ( Aloe vera )
Preliminary evidence suggests that aloe gel used topically may
improve the symptoms of genital herpes. Whether this same use of
aloe will apply to oral herpes lesions is not known, but it may be
worth trying in order to reduce the length and severity of your
symptoms.
Lemon Balm ( Melissa officianalis )
Some studies suggest that topical ointments containing lemon balm
may help heal herpes cold sores. In one study of 116 people with HSV,
for example, those who applied lemon balm cream to their lip sores
experienced significant improvement in redness and swelling after
only two days. Although other symptoms (such as pain and scabbing)
did not improve, both the participants and their physicians reported
that the lemon balm ointment was highly effective. Several animal
studies also support the value of topical lemon balm for oral herpes
lesions.
Peppermint Oil
In test tubes, peppermint oil has exhibited antiviral properties
against a number of infectious agents, including herpes. Whether
this would translate into help for relieving herpes lesions is not
known at this point.
Sage-Rhubarb Cream
In one Swiss study, a cream made from sage ( Salvia officinialis )
and rhubarb ( Rheum palmatum ) lessened the length of time that
herpes lesions were present to the same extent as the medication
acyclovir. More research on this topic would be helpful.
Siberian Ginseng ( Eleutherococcus senticosus/Acanthopanax
senticosus )
Although not all studies agree, one 6-month study of 93 people with
HSV-2 (which, again, generally causes genital herpes lesions) found
that Siberian ginseng reduced the frequency, severity, and duration
of outbreaks. This herb should not be given to children and should
not be taken if you have high blood pressure, obstructive sleep
apnea (repeated, prolonged periods when breathing stops while
sleeping), narcolepsy (frequent day time sleeping), are pregnant or
breastfeeding.
Tea Tree Oil ( Melaleuca alternifolia )
Use of tea tree oil, applied topically in gel form, has some
popularity for herpes lesions on the lips. Although more research is
needed before definitive conclusions can be drawn, there is some
scientific basis for this use. First, in test tubes, tea tree oil
has the ability to fight both strains of herpes viruses (HSV 1 and
HSV 2). Secondly, there has been one small study comparing use of
tea tree oil gel to placebo in those with recurrent oral herpes. The
herpes lesions of those who used the tea tree oil healed more
quickly than those who used placebo. Studies of larger numbers of
people are necessary, however, along with studies that compare tea
tree oil to medications used for herpes.
Others
Additional herbs that may be recommended by an herbal specialist for
the treatment of either oral or genital herpes include:
Pau d'Arco ( Tabebuia avellaneda )
Although Echinacea (coneflower) has gained some popularity for the
prevention of herpes, there is no scientific evidence that it works
for this purpose. In fact, despite test tube studies suggesting that
Echinacea has the ability to fight the herpes virus, one study of
people with herpes did not show any reduction in the number of their
outbreaks.
*To try to prevent herpes outbreaks. Herbalists may also consider
remedies that help strengthen your immune system or act as adaptogens (substances that help relieve stress).
* abstaining
entirely from sugar, chocolate, caffeine, dairy, alcohol, hot/spicy
food, anything processed
* avoiding sex, biking, and other topical irritants and avoiding all
forms of stress which further antagonizes the nervous system
* lots of sleep and rest
Acupuncture
Case reports in the scientific literature suggest that acupuncture
may help reduce the length of time of a herpes outbreak and decrease
your chances for recurrent lesions. Additional research would
be helpful. Acupuncture is used to increase immunity (working to
support remission with the liver divergent meridian). You can also use
carrot oil on Liver DM points.
Massage and Physical Therapy
Regular massage can help alleviate chronic stress; therefore, in
theory, receiving massage on a regular basis may help avoid
recurrent outbreaks. Aromatherapy and using essential
oils during massage therapy has been evaluated for these purposes and results
thus far suggest that this is a useful technique.
Homeopathy
Although few studies have examined the effectiveness of specific
homeopathic therapies, professional homeopaths may consider the
remedies described below for the treatment of herpes based on their
knowledge and experience. One study of 53 people with genital herpes
did show that the majority experienced improvement in their symptoms
and were less likely to have recurrent outbreaks when treated with
homeopathy. Participants in this study were followed for up to 4
years.
Before prescribing a remedy, homeopaths take into account a person's
constitutional type. A constitutional type is defined as a person's
physical, emotional, and psychological makeup. An experienced
homeopath assesses all of these factors when determining the most
appropriate remedy for each individual.
For lesions around the lips and mouth:
Natrum Muriaticum -- for eruptions at the corners of the mouth that
occur during periods of emotional stress and tend to worsen in the
daytime
Rhus toxicodendron -- for eruptions consisting of many small
blisters that itch intensely at night
Mercurius -- for children who drool and may have a fever
Sepia -- for outbreaks that do not improve with other homeopathic
remedies; this remedy is most appropriate for individuals who tend
to have a lack of energy and don't tolerate cold weather
For genital lesions:
*Graphites -- for large, itchy lesions in individuals who are
overweight
*Natrum Muriaticum -- for eruptions that occur during periods of
emotional stress and symptoms that tend to worsen in the daytime
*Petroleum -- for lesions that spread to anus and thighs; symptoms
tend to worsen in winter and improve in summer
*Sepia -- for outbreaks that do not improve with other homeopathic
remedies; this remedy is most appropriate for individuals who tend
to have a lack of energy and don't tolerate cold weather
_______________________
Every
person will respond differently to both the Herpes Virus as well as
the treatments. I hope this information lifts abit of the
mystery surrounding it, if only a little. We grow in knowledge
by continuing to study and studying together builds wisdom!
I can think of more wonderful topics to immerse myself in during
this Blessed Christmas season, but it has been ever so interesting!
~Susan Oshel~
Bibliography:
Maternity and Gynecologic Care, 4th Ed. Pages 851-859
Maternity & Woman's Health Care, 8th ed. Lowdermilk, Perry
Pages 199-210, 1068-1069
Mosby's Medical Dictionary, 3rd ed. Page 893
Taber's Cyclopedic Medical Dictionary, 17 ed. Pages 400, 421,
564, 565, 622, 662, 711
Dr. Sears, The Baby Book Page 710
Dr. Sears, The Pregnancy Book Pages 290, 296-297
Wikipedia, the free encyclopedia
http://en.wikipedia.org/wiki/Herpes_simplex_virus
National Institutes of Health | Department of Health & Human
Services
http://www.nlm.nih.gov/medlineplus/herpessimplex.html#cat27
2007 University of Maryland Medical Center
http://www.umm.edu/altmed/articles/herpes-simplex-000079.htm
International Herpes Alliance
http://www.herpesalliance.org/resources_04.htm
Herpes.com
http://www.herpes.com/pregnancy.shtml
Center For Disease Control and Prevention (CDC Herpes Guidelines
2006)
http://www.cdc.gov/std/treatment/2006/genital-ulcers.htm
American Social Health Assn
http://www.ashastd.org/herpes/herpes_learn_pregnancy.cfm
Written by Susan Oshel, CPM
|